This article is a guideline only and should not be construed as medical advice. Always contact your eye care doctor with questions and for treatment options.
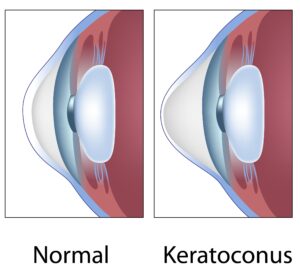 Keratoconus is a progressive eye condition that affects the cornea, which is the clear, dome-shaped front surface of the eye. In individuals with keratoconus, the cornea gradually thins and bulges into a cone-like shape instead of maintaining its normal round curvature. This abnormality can lead to distorted vision and visual impairment.
Keratoconus is a progressive eye condition that affects the cornea, which is the clear, dome-shaped front surface of the eye. In individuals with keratoconus, the cornea gradually thins and bulges into a cone-like shape instead of maintaining its normal round curvature. This abnormality can lead to distorted vision and visual impairment.
Causes of Keratoconus
The exact cause of keratoconus is not well understood, but it is believed to involve a combination of genetic, environmental, and hormonal factors. The condition typically starts during adolescence or early adulthood and progresses over time. Several factors may contribute to the development of keratoconus. These include:
- Genetics: A family history of keratoconus increases the risk.
- Eye Rubbing: Constant rubbing of the eyes may contribute to corneal thinning.
- Connective Tissue Disorders: Conditions such as Ehlers-Danlos syndrome may be linked to keratoconus.
- Environmental Factors: UV light exposure and oxidative stress may play a role.
How Keratoconus Affects Daily Life
How keratoconus affects daily life can vary from person to person, but some common effects include:
- Visual Distortions: Keratoconus often causes blurred and distorted vision. Straight lines may appear wavy, and individuals may experience multiple images, ghosting, or halos around lights.
- Frequent Changes in Prescription: Due to the progressive nature of keratoconus, individuals may experience frequent changes in their eyeglasses or contact lens prescriptions. Adjustments may be needed to maintain optimal vision.
- Sensitivity to Light: Some people with keratoconus may become more sensitive to light (photophobia), making it uncomfortable to be in bright or harsh lighting conditions.
- Difficulty with Night Vision: Reduced contrast sensitivity and increased glare can make driving or navigating in low-light conditions challenging for individuals with keratoconus.
- Eye Strain and Fatigue: Constantly adjusting to changes in vision can lead to eye strain and fatigue, especially when trying to focus on tasks like reading or using digital screens.
- Reduced Visual Acuity: In advanced stages of keratoconus, visual acuity may be significantly reduced, impacting overall quality of life and making activities such as driving or recognizing faces more difficult.
Recognizing the Symptoms
Early detection of keratoconus is essential for effective management. Pay attention if you have:
- Blurred or distorted vision
- Increased sensitivity to light
- Frequent changes in prescription glasses or contact lenses
- Difficulty with night vision
- Eye irritation and swelling
Diagnosis and Screening
Eye care doctors use various diagnostic tools, such as corneal topography and tomography, to assess and diagnose keratoconus. Regular eye screenings are crucial, especially for those with a family history of the condition, to detect and manage it at an early stage.
Treatment Options
The management of keratoconus depends on the severity of the condition. Treatment options include:
- Glasses or Contact Lenses: Initially, in the earlier stages, individuals may use glasses or contact lenses to correct vision.
- PROSE treatment or Scleral Lenses: A non-surgical option for keratoconus, scleral lenses provide unparalleled comfort and visual acuity. These custom-fit lenses vault over the cornea, resting on the sclera (the white part of the eye), creating a smooth optical surface that compensates for the irregular shape of the cornea. PROSE treatment may be necessary in more severe cases of keratoconus.
- Corneal Cross-Linking: This minimally invasive procedure strengthens the cornea and has high success rates to effectively halt the progression of keratoconus.
- Intacs: These are small plastic inserts implanted into the cornea to reshape it and improve vision.
- Corneal Transplant: In severe cases, a corneal transplant may be necessary to replace the damaged cornea with a healthy donor cornea.
Management of Keratoconus
Early diagnosis and intervention can significantly improve the prognosis and quality of life for those dealing with keratoconus. It’s important to work closely with your eye care doctor to find the most suitable solutions for your visual needs and maintain a good quality of life. Regular eye exams are critical to vision improvement when managing keratoconus.